Osteochondrosis is a chronic disease of the spine. It develops with age and consists of degenerative-dystrophic changes that occur in the intervertebral discs. For a long time there have been no symptoms of any kind. A person may only notice some stiffness in the spine.
Osteochondrosis progresses slowly: many factors influence the rate of the disease. If the pathology is not treated, complications arise: sciatica, sciatica and others, depending on the spine. Some doctors believe that such a disease as osteochondrosis does not exist, and only those who do not understand human physiology make such a diagnosis.
Causes
In the 21st century, the disease, compared to the 20th century, has significantly rejuvenated. Quite often you can meet young people who have degenerative-dystrophic changes in the intervertebral discs during a medical examination for another pathology. There is only one reason for this: urbanization and progress.
Today, a person does not need to make an effort to go to work or to get food. Most lead a sedentary lifestyle, eat malnourished and rapidly gain weight, walk in the fresh air and active activities prefer a computer and a comfortable sofa. Even before work, many get into their cars, which are located in the underground garage on the territory of a multi-storey building, and sit in the workplace for 7-9 or more hours.
On a note. Osteochondrosis is just a human disease. None of the mammals had such a pathology. You must understand that this is Homo sapiens' punishment for walking upright.

What causes osteochondrosis?
The following factors can push the onset of the disease against the background of physical inactivity, lack of sufficient physical activity and an unhealthy lifestyle:
- violation of mineral and vitamin metabolism;
- a large number of transferred infectious diseases;
- chronic stress, depression;
- sudden movements, heavy lifting;
- spinal injury;
- severe hypothermia;
- sloppy;
- unnoticed over time and untreated curvature of the spine;
- long stay in an uncomfortable position (not necessarily sitting).
On a note. Great sports have a negative impact on human health. For example, weightlifting (and not only) in the future can become a trigger for degenerative-dystrophic changes of the intervertebral discs.
What happens to the spine?
The following factors directly affect back health:
- blood circulation in the paravertebral tissues is disturbed, the intervertebral discs suffer from a lack of nutrients (they do not have their own blood vessels and depend on the tissues surrounding them);
- the muscular corset that supports the spine weakens, the vertebrae receive an additional load that they cannot withstand;
- intervertebral discs lose moisture, decrease in volume and diameter - the spine seems to sag (many people notice that they become 5 or even 10 centimeters lower with age);
- there is instability of one or more parts of the spine;
- the body solves the problem of instability by making osteophytes grow: these are marginal bone growths which, over time, firmly cement the spine, depriving it of flexibility.
On a note. The transformation of the spine itself does not cause pain: the pain syndrome appears when the nerve roots, large arteries and lymphatic vessels are violated by osteophytes or the anatomical position of the vertebral bodies is changed.
Symptoms
The signs of osteochondrosis increase with the progression of the disease. There are 4 stages of the pathology:
- First. Symptoms are completely absent. No pain. A person may experience a little more fatigue than usual, a certain stiffness of the spine, which he explains to himself with fatigue, excessive physical exertion and overwork. Osteochondrosis in the first stage can be
- According to. A persistent pain syndrome appears due to the violation of the nerve roots, which is easily stopped by non-steroidal anti-inflammatory drugs. If the patient continues to ignore the signals of his body and does not go to the doctor, the disease progresses rapidly. The flexibility of the spine is reduced, especially in the cervical and lumbar region. The onset of vertebral artery syndrome is likely due to its compression by edematous paravertebral tissues or a displaced vertebra.
- Third. Pathology in a state of decay. Pain haunts a person around the clock, slightly weakening in a horizontal position, but it is impossible to stay in one position for a long time (on the back, on the side). Sleep is disturbed, the patient becomes irritable. A person bends over (thoracic, lumbar), looking for a more comfortable position that does not cause discomfort, which becomes an impetus for the formation of hump, scoliosis and other deformities of the spine.
- Fourth. There is an accretion of osteophytes - stabilization of the spine. The patient can only look around by fully rotating the torso. The pain is strong, constant, completely removed only by blocks (novocaine, prednisolone). Disability in the fourth stage is about 80%.

Simultaneously with the listed signs, the patient may be tormented by symptoms that, at first glance, have nothing to do with the back: dizziness, flies in the eyes, arterial hypertension, numbness of the upper limbs (cervical osteochondrosis), chest pain mimicking an attack of angina or cardiac intercostal neuralgia (thoracic osteochondrosis), cauda equina syndrome, numbness of the lower limbs (lumbosacral osteochondrosis).
On a note. The pathology causes vegetovascular and neurodystrophic disorders.
Diagnostics
To establish an accurate diagnosis, the patient is sent for x-ray, myelography and neurological examination of reflexes. If that's not enough, a referral is issued to:
- MRI (magnetic resonance imaging);
- CT (computed tomography);
- NMR (nuclear magnetic resonance).
The doctor also interviews the patient and conducts a medical examination, which reveals areas of pain, possible curvature of the spine, difference in leg length, and other objective signs of damage to the spine.

Therapy
Treatment of osteochondrosis is complex. To stop the degeneration process, or at least slow it down, the following are assigned:
- chondroprotectors - externally, orally (orally), in injections to restore cartilage tissue;
- muscle relaxants - relax spasmodic muscle groups, are used only under medical supervision;
- pain relievers;
- blockages - relieves pain for a long time, but does not cure;
- physiotherapy (magnetotherapy, phonophoresis, vibrotherapy, EHF and others);
- physical therapy and author's gymnastics;
- massage;
- acupuncture;
- balneotherapy and mud therapy.
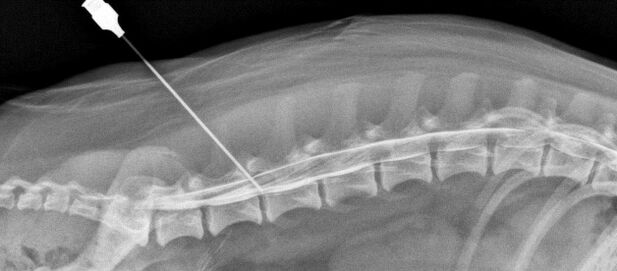
In advanced cases (uncontrolled urination and defecation, cauda equina syndrome), surgery may be required to decompress and stabilize the affected spinal segments.
Rear Access Decompression Operations:
- facetectomy;
- foraminotomy;
- laminectomy;
- laminotomy.
Front access decompression operations:
- discectomy;
- corpectomy.
To stabilize the damaged segment, spinal fusion is used - the fusion of adjacent vertebrae using a special fixed structure (bars). A bone implant is placed in place of the removed intervertebral disc (bone material is taken from a donor or formed from the patient's own bone).

On a note. Spinal fusion can be avoided. Surgeons have achieved a great deal in the surgical treatment of osteochondrosis. Instead of a removed intervertebral disc, it is possible to install an artificial one and thus avoid complete immobilization of the segment. Operations on the spine are fraught with many complications, so they are prescribed only in extreme cases.
Prevention
Hippocrates also said: "It is easier to prevent a disease than to cure it". This rule also applies to osteochondrosis. It is enough for a person to monitor their health, lead an active lifestyle, eat properly, exercise regularly to maintain the health of the spine.

If the disease has still manifested itself, then prevention will help not to start it. Follow these guidelines:
- Sleep on the right mattress and pillow. Choose the orthopedist and consult your doctor first.
- Make it a rule to walk at least half an hour before and after work. During the break, don't sit at the computer or phone, but warm up and then have a snack.
- Watch your weight. The higher it is, the harder it is for the spine.
- Observe the rest mode (work during the day, sleep at night).
- Try to eliminate stress from your life. If you feel you are falling into depression, consult a specialist.
On a note. Traditional healers claim that osteochondrosis can be cured with the help of medicinal herbs. It is difficult to say how true this statement is. Treatment with alternative methods can be used in conjunction with that prescribed by the doctor. Otherwise, the result is not guaranteed.
Osteochondrosis is a dangerous disease, fraught with disability if treatment is not started on time. If you feel that you have tired suspiciously and quickly and in the morning your spine is less flexible than before, see a doctor and undergo a full examination. In the early stages, the pathology can be slowed down and even stopped completely.


























